Section 2. Avian Influenza and Humans
| Sitio: | Extension Foundation Online Campus |
| Curso: | Avian Influenza Biosecurity for Youth and 4-H Members |
| Libro: | Section 2. Avian Influenza and Humans |
| Imprimido por: | Invitado |
| Día: | lunes, 2 de marzo de 2026, 22:15 |
Descripción
1. People and AI
2. HPAI H5N1
3. Bird Migration
4. AI in the US
5. Protecting Yourself
6. Clinical Signs in People
Learning Objectives
We hope that by the end of section 2, that you will understand how the avian influenza virus affects people and how to prevent infection.
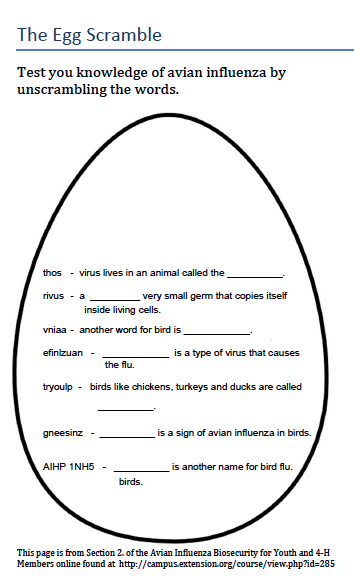
Can I Catch Avian Influenza From Sick Birds?
- Avian influenza (AI) viruses generally do not make people sick; however, cases of human infection have been reported.2
- Most human infections result from direct contact with fluids of infected poultry (e.g. saliva, nasal secretions, and feces) to the person's mucus membranes (e.g. eyes, nose, and mouth). Always wash your hands properly after handling poultry, especially before you eat or touch your face.
- Spread of AI virus from person to person is very rare.
- Poultry should be cooked to 165°F and cooked eggs should have no runny yolks.7

Bird Flu - Highly Pathogenic Avian Influenza (HPAI) H5N1
Bird flu specifically refers to the HPAI H5N1 strain that has killed millions of birds.
HPAI H5N1 is also one of the few avian influenza viruses that can infect humans. Found in Hong Kong in 1997, it has made the most people sick from an avian influenza virus.1
As of June 13, 2016, HPAI H5N1 has been found in 16 countries throughout Asia, Africa, Middle East, and Europe. 851 people have been infected since 2003 and 450 of those people have died. The virus has killed over half (53%) of those infected.4
| World Health Organization - Confirmed Human Cases of HPAI H5N1 (2003-2013) |
 |
| © WHO 2016 |
Bird Migration
|
HPAI H5N1 has not been reported in the United States, however, it is possible that bird flu could enter the country by migratory birds. In order for H5N1 to enter the United States, infected wild birds from Asia or West Africa would have to survive the disease and carry it to breeding grounds in the Pacific Islands, Alaska, or Canada. The virus would then have to pass to another species that migrates to the continental United States.6 Ninety-nine percent of North American migratory waterfowl do not come from Europe, Asia, or Africa where the virus has been found. Scientists continue to test birds in Alaska and Canada and along major flyways in the United States to look for AI. HPAI H5N1 has not been found along major flyways in the continental United States. |
Avian Influenza Outbreaks in the U.S.
While HPAI H5N1 has not been reported in the U.S., outbreaks of other HPAI subtypes have occurred throughout the country.2 To date, there have been four outbreaks in the U.S. of HPAI occurring in 1924, 1983, 2004, and 2014. Several low pathogenic outbreaks have resulted in mass depopulations of poultry as well. Many of these cases are believed to have resulted from contact with AI-infected live bird markets and sharing equipment between farms. |

|
The 2014-2015 outbreak of high pathogenic avian influenza is the largest animal health emergency in US history. In less than six months, over 48 million birds on 223 premises were affected by the virus. The outbreak devastated the affected regions of the Pacific Northwest and Midwest. While the exact cause of the spread from farm to farm has yet to be determined, most experts agree that movement was a major factor. Because the virus can survive in the environment for long periods of time, the virus can be moved from farm to farm by people, animals, farm vehicles or other pieces of equipment. Because of this, biosecurity on individual farms is extremely important and it is imperative to always follow a strict management and health program. Biosecurity includes procedures that minimize risk of a virus or other infectious agent from entering a premise or facility. The following video will provide tips to improve your personal biosecurity.
Documented HPAI in Poultry6,22
| Year |
Location |
Strain |
Losses |
| 1924-25 |
USA |
Unknown |
Unknown |
| 1983-84 |
PA, USA |
H5N2 |
17 million |
| 2004 |
TX, USA |
H5N2 |
9,000 |
2014-2015 |
USA |
H5N2, H5N8, H5N1 |
49 million |
Documented LPAI in Poultry6,22
| Year |
Location |
Strain |
Losses |
| 1978-1995 |
MN |
Various LPAI |
1199 Farms |
| 1995 |
MN | H9N2 |
178 Farms |
| 1995 |
UT |
H7N3 |
2 million (60 Farms) |
| 2002 |
VA |
H7N2 |
4.7 million (197 Farms) |
| 2004 |
DE, MD, PA |
H7N2, H2N2 |
400,000 |
Protecting Yourself
Keep in mind that human AI infections are very rare and using everyday biosecurity precautions are the first step to prevention.
- Use gloves when handling sick or dead birds.
- Avoid contact with droppings and do not touch your mouth or eyes with your hands while working.
- After handling sick or dead birds, change and launder your clothes and always wash your hands with soap and water or gel sanitizer when done.7
- Get your seasonal flu shot. While the seasonal flu will not prevent AI infections, it will help prevent mutant variants from forming. For example, if you are infected with two different virus types they could combine to produce a more infectious strain. Seasonal flu vaccines are inexpensive and offered at many local clinics and pharmacies generally from October to April. Click here to see the 3D4medical virus mutation video.
In 2007, the FDA approved an avian influenza vaccine against one strain of HPAI H5N1 for humans; however, it is not currently available to the public. In the event of a pandemic, the government will distribute the vaccine as needed. |
 CDC Photo Library: Jim Gathany
|
Signs and Symptoms of AI in People
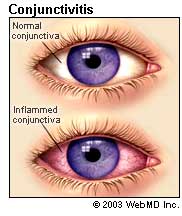 |
- Conjunctivitis (eye infection)2
- Influenza-like symptoms (e.g. fever, cough, sore throat, muscle aches)
- Severe respiratory illness (e.g. pneumonia, acute respiratory distress)
- Occasionally, nausea, diarrhea, and vomiting are seen
Having these signs and symptoms does not mean that you have avian influenza. Human infection with AI is rare and laboratory tests are used to diagnose avian influenza infection.7